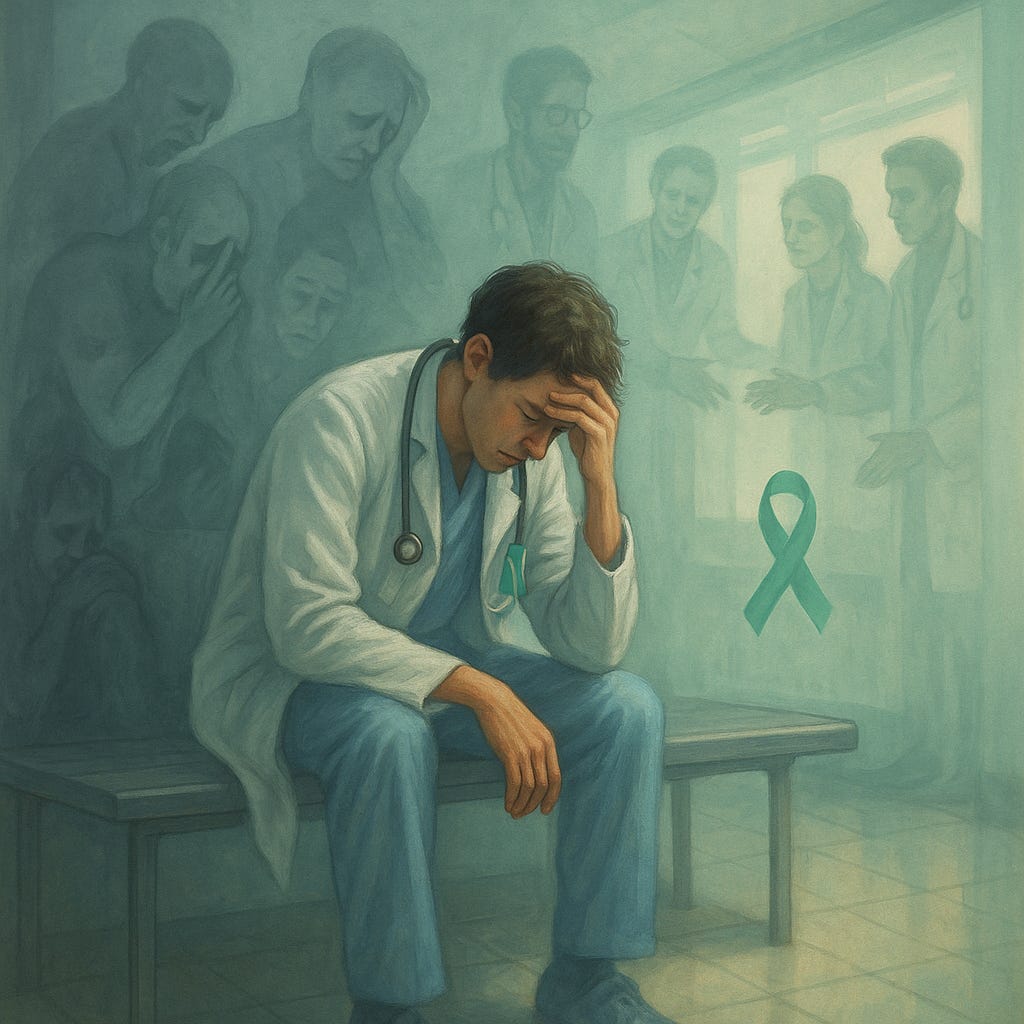
We Don't Talk About Burnout: When Mental Health Feels to Risky to Name
Mental Health Awareness Month
Every May, academic medicine renews its commitment to mental health.
We circulate wellness flyers, encourage people to “ask for help”, and maybe even host a mindfulness workshop or two.
But let’s be honest: in many training environments, the real message is still this:
“Say you’re struggling and your competence might be questioned”.
As someone who has spent years working alongside residents, fellows, and faculty, I can tell you this: burnout isn’t always loud. It doesn’t always look like breakdowns or missed deadlines.
Sometimes it looks like:
The intern who worked through their vacation and hasn’t smiled in weeks.
The PGY-3 who stays late. Not to learn, but because they’re terrified of being labeled “unreliable”.
The attending who was told they were “too emotional” for speaking up during rounds.
The person praised for being “so resilient”, who’s silently running on fumes.
Let’s Talk About What’s Not Working
Too often, wellness efforts focus on the individual:
”Practice mindfulness”
”Take a break”
”Use the employee assistance program”
But real burnout is about systems, not just stress.
It’s what happens when high standards meet low support-on repeat.
The truth is, many people do not trust the systems designed to help.
They fear retaliation.
They fear judgement.
They fear what might happen to their career if they speak up.
What if We Focused on the Environment, Not Just the Individual?
This Mental Health Awareness Month, I’m inviting GME leaders to consider a different kind of strategy:
Create environments where mental health is protected by culture, not just policy.
That means zooming out from individual coping strategies and asking more systemic questions.
Mini Reflection Worksheet: Signals & Systems:
Use this 5 question tool with your team to start the conversation:
1. What signs of burnout are showing up in your team?
☐ Emotional exhaustion
☐ Cynicism or disengagement
☐ Reduced sense of accomplishment
☐ Silence during feedback or evaluation
☐ High levels of performative “resilience”
2. Where is burnout being treated as a personal failure rather than a systemic red flag?
What messages spoken or unspoken exist around exhaustion or struggling?
3. What’s one structure, policy, or norm that might be unintentionally contributing to burnout?
Think: Scheduling? Supervision? Feedback culture?
4. Who has psychological safety to speak up—and who doesn’t?
What would it take for more people to feel safe naming stress, overwhelm, or mental health concerns?
5. What’s one micro-change your team could make this month to create a more supportive environment?
(Even if you can’t change the system overnight, you can shift the tone.)
Let’s Stop Pretending We’re Fine
If we want to improve mental health in medicine, we can’t just offer tools.
We have to build cultures that make people feel safe enough to use them.
So this month, instead of offering more “wellness week” suggestions, I’m encouraging leaders to:
Look Deeper. Rebuild Trust. Start small-but stay real.
Let’s stop asking people to prove they’re strong by staying silent.
Let’s build systems that prove we’re listening.
With care,
Sophia Gilmore, EdD, MPA, TAGME
Founder MedEd.Lead| GME Strategist | Educator